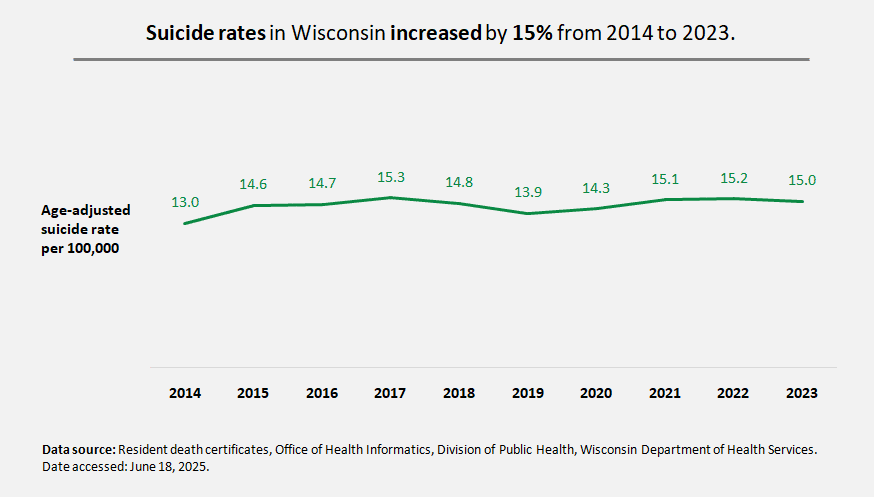
The age-adjusted suicide rate in Wisconsin increased by 15% from 2014 to 2023.
In 2022, the national age-adjusted suicide rate was 14.2 per 100,000, while Wisconsin’s age-adjusted rate was higher at 15.2 per 100,000 (Source: CDC Suicide Data and Statistics, accessed 6/18/2025).
In 2023, suicide was the 8th leading cause of death for all Wisconsin residents and the 2nd leading cause of death for youth 5-25 years old (Data Source: DHS Leading Causes of Death Dashboard, accessed 6/18/2025).

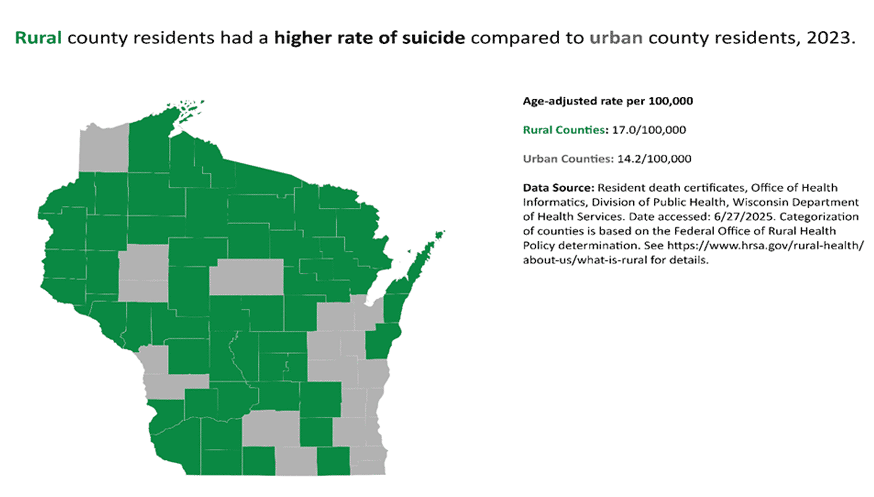
Suicide rates vary across the state by geographic location. In 2023, suicide rates were significantly higher for residents living in rural counties, 17.0 per 100,000, compared to Wisconsin residents living in urban counties, 14.2 per 100,000. Urban counties include Brown, Calumet, Chippewa, Dane, Douglas, Eau Claire, Fond du Lac, Kenosha, La Crosse, Marathon, Milwaukee, Outagamie, Ozaukee, Racine, Rock, Sheboygan, Vernon, Washington, Waukesha, and Winnebago. All other counties are rural.
Social determinants of health like access to services, built environment, and cultural attitudes around mental health and help-seeking can vary from place to place. These conditions can promote protective factors or produce risk factors for suicide. In rural areas, residents may be more likely to face stressors like social isolation, economic hardship, stigma, and barriers to care, including lack of broadband internet which makes it harder to access telehealth services (Rural Health Information Hub).
In Wisconsin, sex data related to suicide is limited to the categories of male and female. Sex refers to biological and physical characteristics of the reproductive system, while gender refers to one’s identity as it relates to socially constructed roles. The data available provide an incomplete picture of the gender spectrum and do not fully reflect identities held by those who died by suicide. Advocacy and training are needed to improve the accuracy of data collected on suicide among gender non-conforming populations.
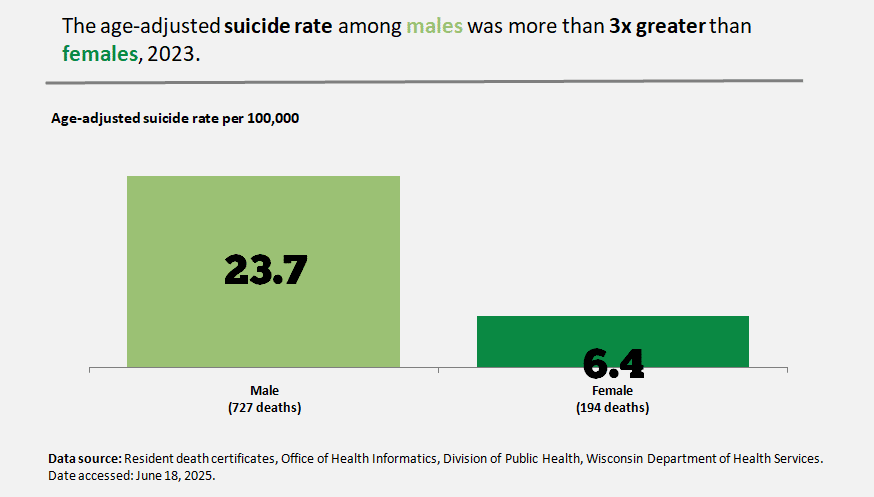
In 2023, Wisconsin males died by suicide at a disproportionately higher rate, 23.7 per 100,000, compared to females at 6.4 per 100,000. Males account for almost 80% of all Wisconsin suicides. Of those who died by suicide, men were approximately twice as likely as women to use firearms. In addition to increased access to lethal means, stigma around asking for help, and insufficient social support may impact male suicide rates.
In addition to suicide disparities by sex, there are also disparities by race. When an individual dies by suicide, race and ethnicity data are collected and reported on death records. This information is recorded by a funeral director or person serving in that role. Wisconsin law requires this information be obtained from next of kin or best qualified person or source available (Suicide in Wisconsin Dashboard).

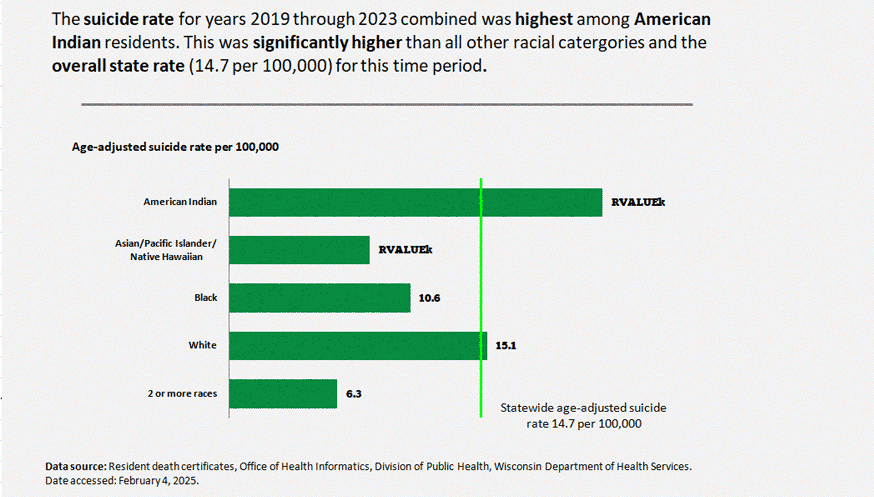
American Indian residents had the highest suicide rate at 21.8 per 100,000 for the combined years 2019-2023. This was significantly higher than all other racial categories and the overall statewide age-adjusted rate (14.7 per 100,000) for the same time period.
White residents had the second highest rate at 15.1 per 100,000.

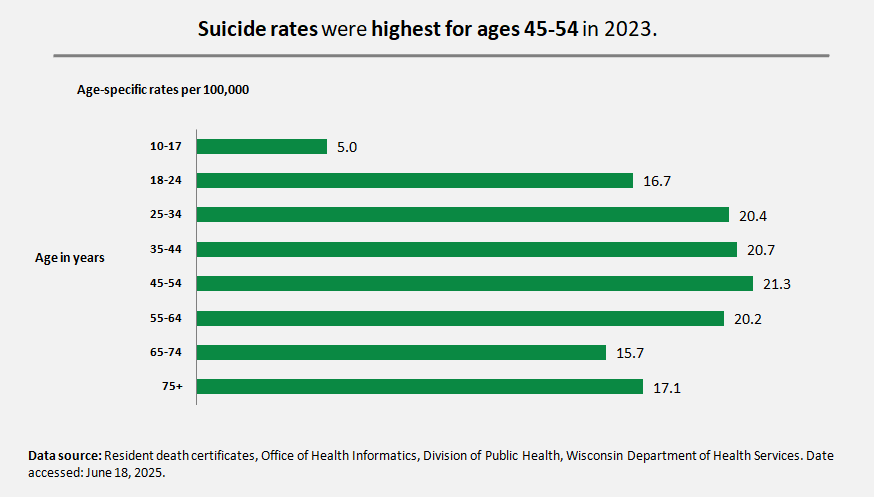
Suicide impacts people across the lifespan. In 2023, suicide rates were highest among those 45-54 years old.
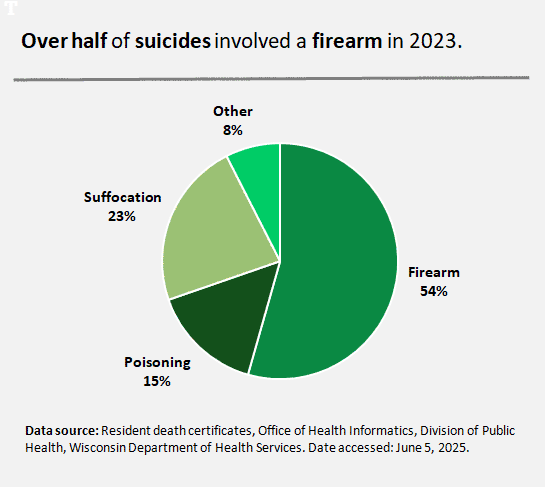 Over half of all suicide deaths in 2023 were by firearm (54%) with suffocation as the next most common method used (23%). Poisoning (which includes medications, drugs, biological and other substances such as cleaning fluids) accounted for 15%. A description of other means, which accounted for 8%, can be found on the Suicide in Wisconsin Dashboard. Firearms are the most lethal method of suicide, and attempts are almost always fatal. Suffocation, poisoning, and other methods listed above may be less immediately fatal and allow valuable time for life-saving intervention to occur.
Over half of all suicide deaths in 2023 were by firearm (54%) with suffocation as the next most common method used (23%). Poisoning (which includes medications, drugs, biological and other substances such as cleaning fluids) accounted for 15%. A description of other means, which accounted for 8%, can be found on the Suicide in Wisconsin Dashboard. Firearms are the most lethal method of suicide, and attempts are almost always fatal. Suffocation, poisoning, and other methods listed above may be less immediately fatal and allow valuable time for life-saving intervention to occur.
Suicide Among Veterans
In 2023, the suicide rate among veterans was 54.9 compared to 17.7 per 100,000 among non-veteran adults. 70.9% of veteran suicides used a firearm compared to 51.5% of non-veteran suicides. Veterans have unique risk factors for suicide, including increased access to firearms, experiences of moral injury, post-traumatic stress disorder, and other service- and non-service-related stressors. In addition, research has shown that nearly 60% of veterans who die by suicide are not enrolled in care with the U.S. Department of Veterans Affairs (VA), revealing an inability to reach veterans in need of support (U.S. Department of Veterans Affairs, 2024).
 Given the unique aspects of veteran lived experience, there is a need to tailor suicide prevention efforts to reach this population. For example, firearm secure storage efforts can be strengthened through partnership with veterans to design and disseminate communications in a way that better aligns with military culture. Peer support among veterans can open space to relate and share experiences navigating VA care, mental health challenges, and other aspects of the veteran experience.
Given the unique aspects of veteran lived experience, there is a need to tailor suicide prevention efforts to reach this population. For example, firearm secure storage efforts can be strengthened through partnership with veterans to design and disseminate communications in a way that better aligns with military culture. Peer support among veterans can open space to relate and share experiences navigating VA care, mental health challenges, and other aspects of the veteran experience.
Suicidal Thoughts and Actions Among Youth
Suicide rates are lowest for Wisconsin youth ages 10-19 years, but as the second leading cause of death for this age group, it is still a significant public health concern. In 2023, the suicide rate for youth ages 10-19 was 6.4 per 100,000. Youth account for the highest rates of emergency department and hospital patients with self-harm. In addition, on a national scale, the suicide rate among Black youth has been increasing faster than any other racial/ethnic group (Ring the Alarm, 2020).
Self-reported data through tools like the Youth Risk Behavior Survey (YRBS) can help uncover factors that may be related to youth suicide, self-harm, and mental health struggles. The 2023 YRBS state sample includes responses from 1,882 students in 42 public, charter, and alternative high schools in Wisconsin during the spring of 2023. Of those students, 19% seriously considered suicide, 15% made a plan to attempt suicide, 9% attempted suicide, and 60% reported at least one mental health concern.
The percentage of students who seriously considered suicide increased by about 40% between 2013 and 2023 (13% to 19% of students).
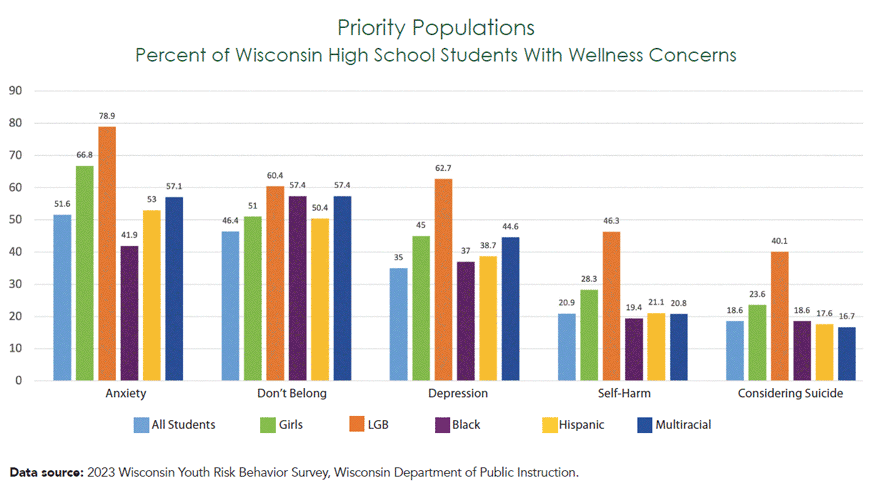
YRBS data reflects that certain populations of students are dealing with significantly more mental health concerns. Lesbian, gay, or bisexual (LGB), Black, Hispanic, and multiracial students report higher rates of suicidal ideation, self-harm, depression, anxiety, and lack of belongingness compared to the average among all students. Girls report these concerns more than boys and more than the average. These data suggest a need to tailor mental health support according to the unique identities and experiences of these students.
Data source: 2023 Wisconsin Youth Risk Behavior Survey, Wisconsin Department of Public Instruction.
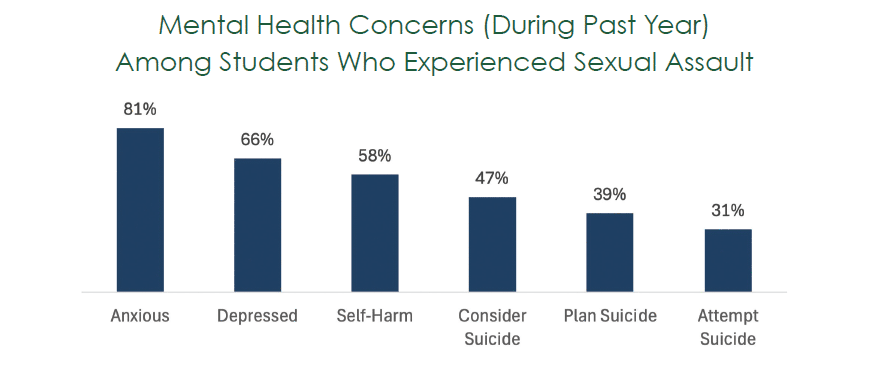
Sexual assault and coercion are also significant drivers of poor youth mental health. Of those students who experienced sexual assault or coercion, 58% self-harmed, 47% considered suicide, 39% made a plan, and 31% attempted suicide. This points to an opportunity to improve youth mental health and prevent suicide through sexual violence prevention efforts and resources to support youth survivors of sexual assault and coercion.
Self-Harm
Self-harm refers to intentional actions taken to hurt oneself. Self-harm may be done as a coping strategy in response to stress, anxiety, or other emotional and/or mental health concerns. Someone who self-harms may or may not have the intention to die by suicide, and injuries resulting from self-harm can range from minor to severe. Additionally, self-harm may refer to current behavior that does not include an initial injury. All instances are a public health concern and may put a person at greater risk for repeated self-harm, suicide attempt, or death by suicide.
Self-harm data are presented separately for Emergency Departments (ED) and hospital patients in this report. Patient type can be used as a proxy for severity. For example, if the injury is more severe, the patient would likely be admitted as a hospital patient instead of treated and released from the ED.
In 2023, the statewide age-adjusted rate of ED patients with self-harm was 60.1 per 100,000 and for hospital patients with self-harm it was 67.5 per 100,000.
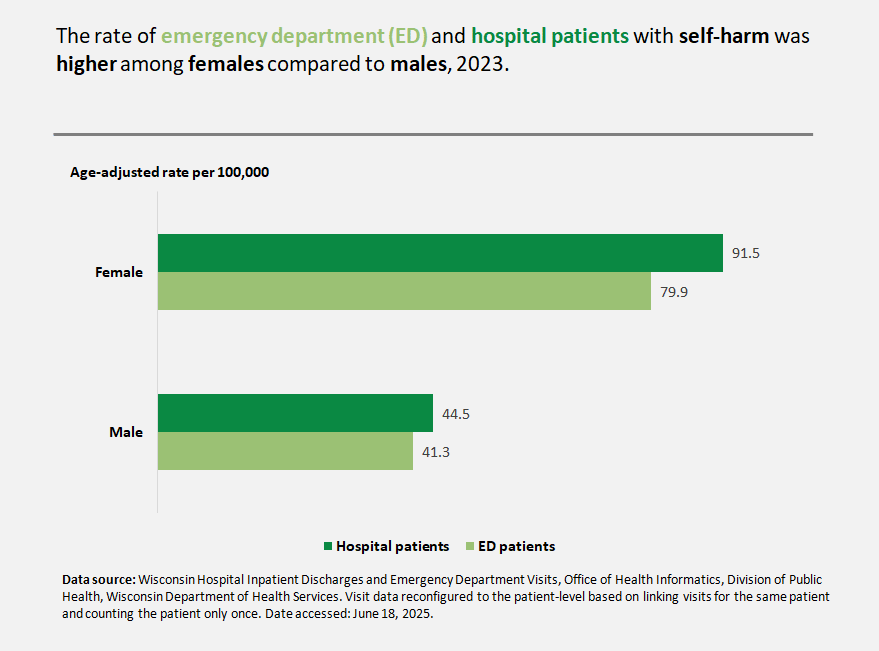
There were significant differences by sex with the rate of ED patients with self-harm among females at 79.9 compared to 41.3 per 100,000 for males. The age-adjusted rate of hospital patients with self-harm among females was even greater at 91.5 compared to 44.5 per 100,000 for males.
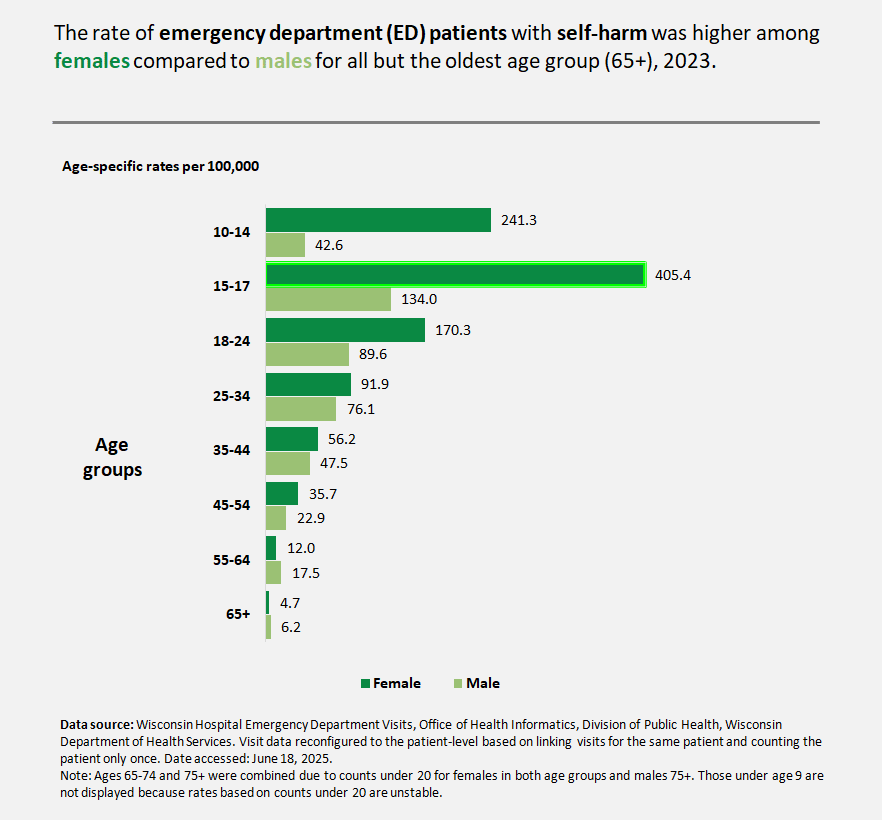
The rate of ED patients with self-harm was highest among females 15-17 years old at 405.4 per 100,000. This was three times greater than for males of the same age. Females 10-14 years old had the second highest rate at 241.3 per 100,000, which was five times greater than males of that age.
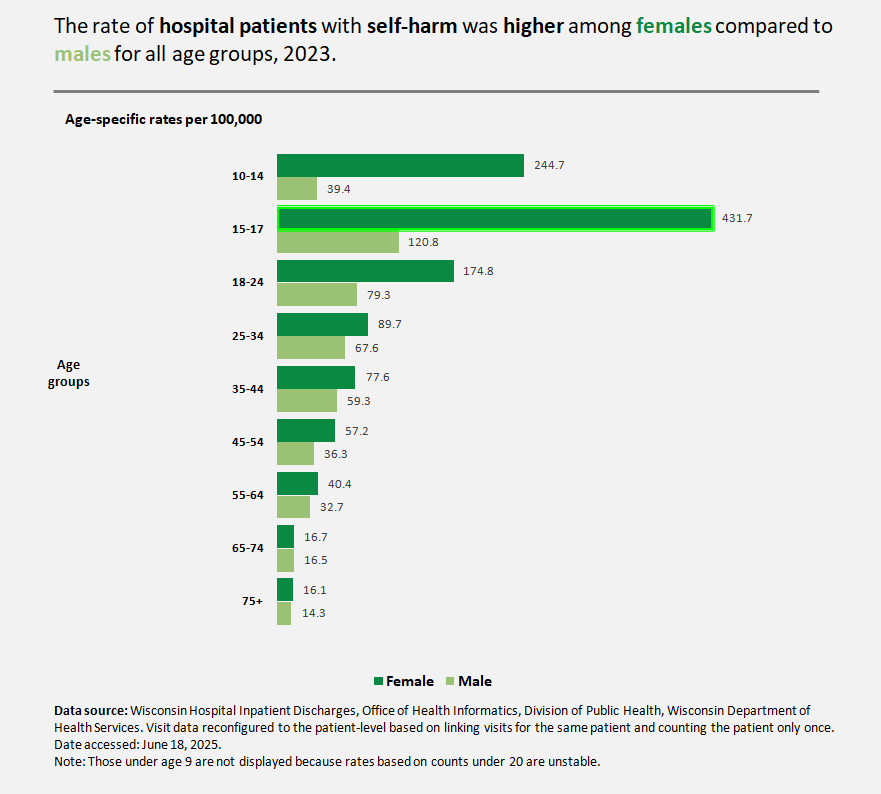
The rate of hospital patients with self-harm was highest among females 15-17 years at 431.7 per 100,000. This was more than three times greater compared to males of the same age. Females ages 10-14 had the second highest rate at 244.7 per 100,000, which was six times greater than males of that age. For males, the 15-17-year-old age group also experienced the highest rates of hospital and ED patients with self-harm.
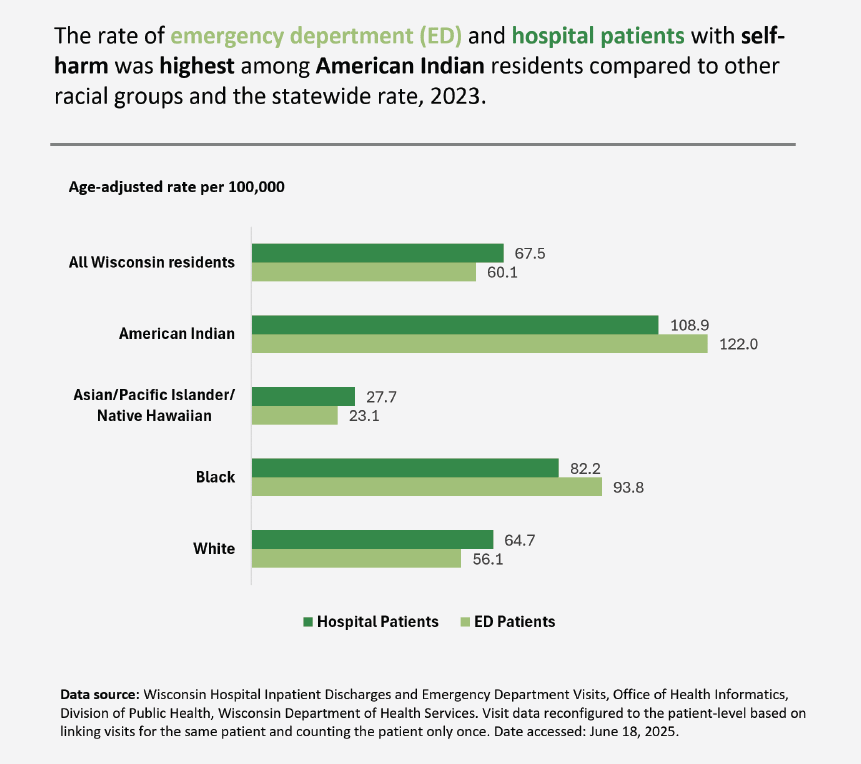
Age-adjusted rates for ED and hospital patients with self-harm were highest among American Indian residents at 122.0 and 108.9 per 100,000, respectively. The age-adjusted rates were second highest among Black residents at 93.8 and 82.2 per 100,000, respectively.
While the Wisconsin suicide and self-harm data shows disparities by age, sex, and race, it doesn’t explain the cause of these disparities. Racism, sexism, and heterosexism (discrimination or bias based on sexual orientation) may impact populations separately or they may compound to increase stress resulting in poor health outcomes that affect some communities more than others. Economic, social, and legal conditions and issues can also drive despair and suffering; these can be intensified by racism, sexism, and heterosexism and negatively influence a person’s health and mental status. Stressors resulting from discriminatory systems may contribute to increased self-harming behaviors among communities harmed by these inequitable systems. Understanding the impact of these structural inequities can support the development of appropriate public health intervention strategies and ensure equitable services for all (Wisconsin Self-Harm Data Dashboard).
Additional Information